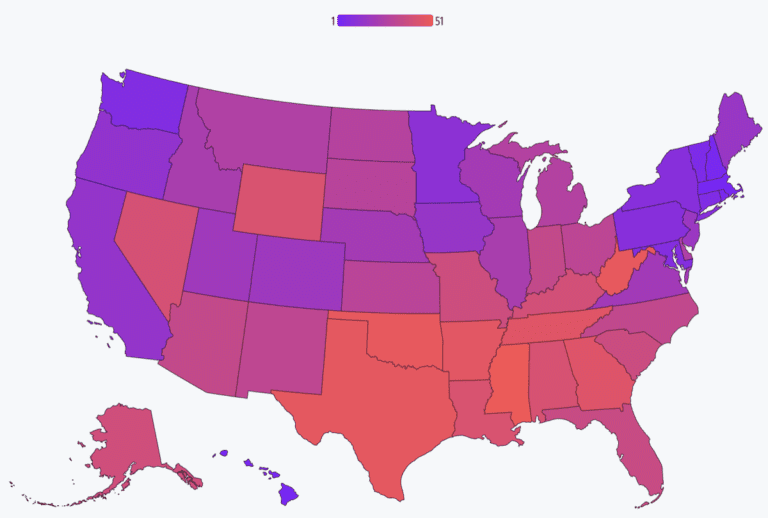
America's best states for health care are mostly in the Northeast, according to new report from the Commonwealth Fund.
Using metrics such as health care access and affordability, preventive care and treatment, potentially avoidable hospital use and costs, healthy living, reproductive care and women's health, income inequality, and racial and ethnic health equity, the Commonwealth Fund ranked all 50 states and Washington. DC using a scorecard based on overall quality of health care.
The top five states were Massachusetts, Hawaii, New Hampshire, Rhode Island, and Vermont, while the bottom five states included Mississippi, Oklahoma, West Virginia, Texas, and Arkansas.
Among the last 10 states, six are between those that have not yet adopted the Medicaid expansion, which greatly improved health care access and affordability.
Non-expansion states also have significantly higher rates of uninsured residents: Texas, one of those states; has the highest percentage of uninsured in the country at 18%.
The state of emergency in the time of the pandemic activated says it enrolls Medicaid recipients on an ongoing basis, but that ended on March 21. about 15 million people expected to lose coverage.
“The losses are becoming apparent as states redefine eligibility for Medicaid enrollees,” Commonwealth Fund vice president for health care coverage and access and monitoring health system performance Sara Collins said on a call with reporters. “To preserve and build on the gains made during the pandemic, we must closely monitor Medicaid relaxation and ensure that those who lose coverage can regain it quickly.”
Maternal mortality and health equity
Reproductive care and women's health also played an important role in the country rankings. (The outcome of the Roe v. Wade overturn occurred in 2022, while the scorecard data expires in 2021.)
The scorecard measured health outcomes for women and infants, including maternal and infant mortality, as well as access to health services such as screening and prenatal and postnatal care. Racial and ethnic disparities were also taken into account.
Jesse Baumgartner, senior research fellow at the Commonwealth Fund, noted that the national maternal mortality rate increased by nearly 40% between 2019 and 2021. During that time, maternal mortality rates have also increased in nearly every racial and ethnic group.
Overall, the maternal mortality rate per 100,000 live births in 2021 was 32.9, but the numbers vary widely by demographic. Among black women, the rate is 69.9, while for American Indian/Alaskan women, the number jumps to 118.7.
Rates also vary by location — between 2019-2021, California's maternal mortality rate was 9.6 while Mississippi's reached 50.3. Other states with high rates include Tennessee, Louisiana and Alabama.
“Many of these deaths could have been prevented through better, more equitable access to comprehensive health care, along with greater efforts to eliminate disparities in the quality of care received,” Baumgartner said on the media call. “This includes health services during and after pregnancy. State variations in care become apparent when we look at specific services.”
For example, she said, nearly 30 percent of women in Texas and Florida did not receive early prenatal care in their first trimester of pregnancy in 2021, while Vermont, the top-performing state, saw only 11 percent of its women receive do not receive early prenatal care. Care.
“Another epidemic that deserves our urgent attention”
As a result of the devastating effects of the coronavirus pandemic on mental health, the number of combined drug overdose deaths, alcoholand suicide — so-called “deaths of despair” reached record levels in 2021.
Part of it is because people can't access mental health care, either as a result of restrictions due to COVID, availability of providers, or other factors like cost.
“We know the ways that COVID-19 has reverberated through all aspects of government health systems, and we're still seeing its impact,” David Radley, a senior scientist at the Commonwealth Fund, said on the call. “We found large increases in early-life deaths from preventable and treatable causes in all states. These increases are due to deaths attributable to COVID-19, but also included increases in drug overdose, suicide and firearm deaths, and even some chronic diseases that have been exacerbated by COVID-related health care disruptions.”
The numbers are alarming for both teenagers and adults. ONE 2020 federal survey by Mental Health America found that 60% of adolescents between 12-17 years of age who had a major depressive episode received no treatment, while 55% of adults with mental illness reported the same. Cost was cited as the main barrier among adults not receiving care.
Drug overdose is also a major problem in the US. More than 106,000 people passed away from drug overdoses in 2021, up 16.2% from 2020.
“There is no doubt that mental health has been underfunded for decades,” explained Dr Joseph Betancourt, president of the Commonwealth Fund. “The impact of the pandemic on mental health has created what I would argue is another epidemic that deserves our urgent attention.”
And “as we think about mental health challenges,” he added, “this is only going to get worse until we make real investments in the behavioral health workforce, integrating behavioral health into primary care and substance use disorder treatment nationwide.”
—
Adriana Belmonte is a reporter and editor covering politics and health care policy for Yahoo Finance. You can follow her on Twitter @adrianambells and contact her at adriana@yahoofinance.com.
Click here for political news about business and money
Read the latest financial and business news from Yahoo Finance