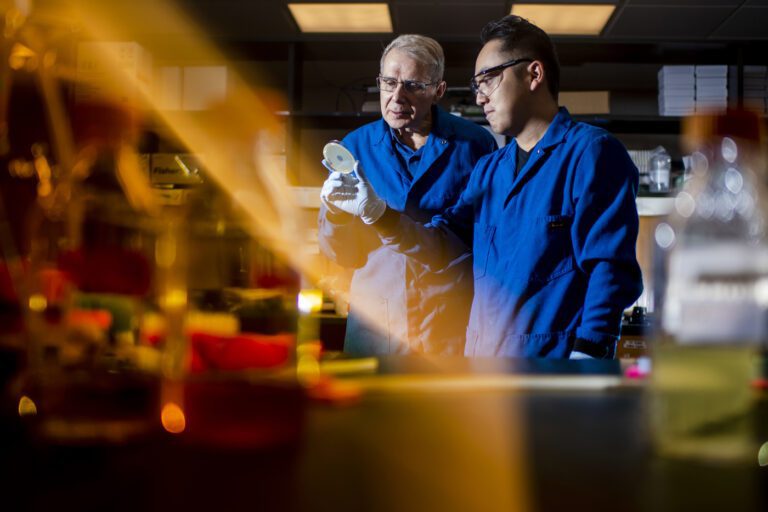
A new antibiotic was discovered by the distinguished Northeastern professor Kim Lewis could be an important new weapon in the growing fight against drug-resistant bacterial infections and superbugs.
Lewis, a microbiologist and director of Northeastern's Center for Antimicrobial Discovery, authored a paper published Tuesday in renowned journal Cell on the discovery and potential of clobibactin, a new antibiotic isolated from a previously uncultured bacterium found in the sandy soil of North Carolina.
Clobibactin blocks the formation of bacterial cell walls by an unusual mechanism. It acts like a glove or cage to wrap around and bind three different phosphate-containing molecules needed to build the wall, according to the researchers.
“It grows like a chain. Once the structure is built, it becomes very strong,” says Lewis. “It's like a Velcro mechanism where every point of the Velcro is weak. But once you have the full Velcro, many, many points that connect together, you have an extremely strong bond.”
“I think this is the end of the road in the evolution to avoid antibiotic resistance,” says Lewis.
The authors of the Cell article call clobibactin “a powerful antibiotic” that “promises to enable the design of improved therapeutics that kill bacterial pathogens without the development of resistance.”
Lewis, who founded NovoBiotic Pharmaceuticals, one of several research groups mentioned in the article, says the problem of increasing antibiotic resistance needs to be addressed.
“According to the World Health Organization, we are in the midst of a pandemic of the antimicrobial resistance crisis. It's a slow-moving pandemic, unlike COVID, but millions of people around the world die every year from multidrug-resistant bacteria.”
“The pipeline is too thin for any realistic chance of antibiotic development,” Lewis says, calling the discovery of clobibactin “a big step.”
“The most important thing about clobibactin, apart from its promise as a breakthrough drug, is that it expands our understanding of antibiotics and what's possible,” he says.
99% of the world's bacteria 'uncultured'
Only about 1% of bacteria in the world are considered “cultivable” and can be grown in a lab to produce antibiotics.
As a result, no significant new antibiotics have been developed since the golden age that began with the development of penicillin in 1943 and extended into the 1960s.
A story published in 2015 detailed how Lewis and Northeastern biology professor Slava Epstein discovered a different bacterium by using diffusion chambers and other technology to “trick” it into growing in the lab.
Developing the bacterium from which clobibactin is derived required a different approach, which Epstein, co-founder with Lewis of NovoBiotic Pharmaceuticals, advocated.
Lewis says that Epstein guessed that some bacteria in soil are dormant and that, given sufficient incubation time, they would begin to multiply as quickly as other bacteria in a Petri dish.
This method was used by NovoBiotic scientists, who incubated a soil sample for three months instead of the usual two days, and one of the cells that eventually grew belonged to a new species, E. terrae ssp. Carolina, from which clobibactin was isolated, Lewis says.
Tourists bring home trinkets. microbiologists, soil
He says it's possible the North Carolina soil sample was picked up by a NovoBiotic employee on his travels or mailed by a relative.
“The diversity of microorganisms changes with geography and soil type,” he says, which is why NovoBiotic employees bring home “souvenirs” from their travels.
Lewis says he was involved in identifying the mechanism of action of clobibactin with Markus Weingarth at Utrecht University in the Netherlands. The study also involved researchers from the German Center for Infection Research and the University of Bonn in Germany.
“This is a new type of mechanism of action,” says Lewis.
“The most exciting thing is that it is unique and binds to an extremely simple target (phosphate molecules) that cannot be changed,” he says, adding that this is why the paper is called, “An antibiotic from an uncultured bacterium binds to an unchangeable target. “
“This is the first discovery of a compound that binds a single, invariant target.”
It awaits over a decade of research
While a variable target lends itself to resistance, Lewis says that in this case the antibiotic binds to the target and then forms long fibrils on the bacterial cell surface, creating “what we call a supramolecular structure.”
So far, clobibactin trials have cleared MRSA infections in mice, which Lewis calls “the gold standard for determining whether your antibiotic is a viable drug.”
The new antibiotic is not toxic to human cells in the lab, but Lewis says development of clobibactin as a therapeutic is a long way off.
If it shows promise at different points along the way, it could take another 12 years to reach the market, he says.
“We are at the first step.”
Cynthia McCormick Hibbert is a reporter for Northeastern Global News. Email her at c.hibbert@northeastern.edu or connect with her on Twitter @HibbertCynthia.